The patient, a forty-four-year-old female, presents with ringing in the right ear. She describes her situation to the doctor using as few words as possible. She hopes to signal, via her narrative concision, that she understands and respects the doctor’s time constraints.
The doctor asks a few follow-up questions. Do you suffer from migraines? Yes, the patient suffers from migraines. Are you dizzy? Not dizzy, the patient says. What she feels more resembles occasional motion sickness.
The doctor looks in the patient’s ear. “You may be in the very early stages of Ménière’s disease. Don’t look it up online,” she says, not joking. “Let’s schedule a hearing test.”
As the receptionist processes the patient’s co-pay, the patient googles “menieres disease” on her phone. Bilateral hearing loss is involved, as are “severe, incapacitating, unpredictable” vertigo that can last for hours and tinnitus that “disturbs your sleep.” Because of its chronic, untreatable nature, the disease is likely to cause stress, anxiety, and depression. Had the patient — who until six months ago had never been sick in her life — not recently been misdiagnosed with interstitial cystitis, a chronic and incurable inflammation of the bladder lining, about which an online sufferer quoted her doctor as saying, “It won’t kill you, but it will make you wish you were dead,” she might have panicked. She might have believed the doctor. As she’d done the last time she’d been given a living death sentence by a medical expert, she might have wept as she walked home through the park. Because she knows better, she does none of these things.
Emily Owens, M.D. is a medical drama that premiered on the CW on October 16, 2012. It was canceled six weeks later. I loved this show. Medical dramas allow me to imagine myself a doctor while underscoring that I don’t need to be one. I can co-solve a bodily whodunit while receiving a psychological IV infusion reassuring me that doctors are emotionally and intellectually and ethically and anatomically fanatical about their patients. They will sacrifice anything — sleep, marriage, the mercurial favor of the vindictive chief resident, the chance to finally hook up with a med-school crush in the supply closet — to correctly diagnose and cure us. They live for our not dying.
The show’s protagonist, a medical intern named Emily Owens, is a listener and an empath. The patients at Denver Memorial Hospital favor her — a mark against her doctorly seriousness, in the eyes of her peers and superiors. In the first (and only) season’s sixth episode, she is sent by the “world-famous pediatrician” and hubristic hospital hottie Kyle Putnam to “play interference” with a worried mother who, Putnam says, “is driving me crazy. So I need you to keep her away from me.” Putnam and Owens enter the hospital room to find the father cradling a sick baby and the baroquely frantic mother cradling a tablet, presumably googling her child’s symptoms. “It could be a heart condition or leukemia or a stroke!” she jabbers.
“This is Dr. Owens,” Putnam says. “She will answer any and all questions you have.” To Owens he whispers, “Bonus points if you can get the mom on meds.” Back in the hallway Putnam soapboxes to Owens, “The Internet has ruined medicine. . . . Medicine should remain inaccessible. . . . You know, we should invent a private language for doctors.”
The selective hearing of doctors, according to Leana Wen and Joshua Kosowsky in their book When Doctors Don’t Listen: How to Avoid Misdiagnoses and Unnecessary Tests, is the result of the growing prominence of the “cookbook medicine” approach to diagnosis and treatment. Cookbook medicine trains doctors to follow “recipes” or “algorithms.” Wen and Kosowsky explain as follows:
[I]f the patient has “chief complaint A,” then ask about risk factors 1, 2, 3. If present, then do a “work up” with tests I, II, III. If negative, then diagnoses x, y, and z can be “ruled out,” so consider additional tests IV, V, and VI.
Doctors, they conclude, are listening, but not to your entire story. They are listening for a “chief complaint” in order to activate a diagnostic protocol.
Wen and Kosowsky examine the case of an “out-of-shape forty-eight-year-old” man who, while moving heavy boxes, experienced tightness in his chest. Worried, the man went to the ER. At the mention of chest tightness, the triage nurse activated the “chest pain pathway.” The man was trussed up in electrodes. This seemed unnecessary to him, given that the tightness was subsiding (and felt like a muscle spasm), but he decided to heed their advice, even though he’d be paying out of pocket for some of his tests. The patient was administered an EKG, a chest X-ray, and multiple blood draws over the course of several hours to check his enzyme levels. He spent the night. In the morning, the patient was administered a stress test. The test proved inconclusive. He was deemed out of shape — and out of danger — and released.
Said this man’s ER doctor: “Does the chest pain pathway get activated more than it should? Probably. Actually, we know that very few, if any, of these patients will ultimately turn out to have heart attacks. But as doctors, we always have to think about the worst-case scenario. A middle-aged, overweight man with chest pain? That’s a heart attack until proven otherwise.”
Wen and Kosowsky diagnose this treatment scenario as follows: “[T]he chief complaint becomes a proxy for the patient’s story, setting in motion a course of action that may or may not have any real relevance for the individual patient.”
After confidently reassuring herself that she does not have a disease — Ménière’s — that afflicts less than half a percent of the population, the forty-four-year-old female patient is dealt a further blow. Though she passes her hearing test, her symptoms, over the next five days, intensify. She experiences painful pressure and popping in her right ear. Both are symptoms of Ménière’s. She develops acute sensitivity to sound. She also becomes unremittingly motion sick. She learns that motion sickness can be alleviated by taking allergy medication. She does this. The motion sickness is managed. She keeps googling. She discovers that a man incorrectly diagnosed with Ménière’s turned out to have a temporomandibular joint (TMJ) problem, and that another wrongly diagnosed Ménière’s patient had a sternocleidomastoid trigger point, the sternocleidomastoid being the muscle that runs down either side of the neck, sometimes forming taut bands of muscle fiber (trigger points) that can cause nausea, popping, and ringing. The patient grows excited. She wakes each morning with a painfully tight right side of her jaw and a sore right molar! Her neck is stiff! All of these symptoms point to a potential TMJ issue. Or at least to the existence of a sternocleidomastoid trigger point.
Because the patient does not want to anger the doctor by appearing to think she knows more or better than the doctor does, she makes no mention of the discoveries she’s made online. She does mention the nausea and the inner-ear pressure. Then she says, as neutrally as possible, “I awake each morning with a tight jaw. My neck is sore. My tooth aches.” The doctor doesn’t seem interested in her jaw, neck, tooth. She says, “Nausea and ear pressure are consistent with Ménière’s.” She gives the patient a hearing test. The patient passes. The doctor says, “Come back in six months; if your hearing has worsened, we can be pretty certain that you have Ménière’s.”
The patient grows frustrated. She breaks doctor-patient etiquette and forthrightly says, “Is it possible this is a TMJ problem?” The doctor says, noncommittally, “It’s possible. But I don’t treat TMJ.” She does not suggest a doctor who does. The patient asks for a recommendation; the doctor mentions the name of a nearby institute. “You can look it up online,” she says.
Wen and Kosowsky, in When Doctors Don’t Listen, reflect nostalgically on what they call the “Golden Age of Medical Diagnosis,” during which there existed a healthy interplay of art and science in the form of the country doctor or the family practitioner. (A similar nostalgia was voiced by the surgeon and television personality Mehmet Oz in a recent New Yorker profile: “I would take us all back a thousand years, when our ancestors lived in small villages and there was always a healer in that village.”) The family practitioner often knew his patients from their infancy, since he (he was usually a he) had delivered them. He made house calls; he understood the physical and familial context of every illness. Write Wen and Kosowsky, “Older doctors frequently bemoan the fading emphasis on the art of medicine,” eager to return to a time when patients had a familiar GP nearby and “were confident that someone who cared about them was listening to their story.”
Wen and Kosowsky compare algorithmic — “cookbook” — medicine to a detective who solves a murder by focusing on a single suspect in order to prove he is not the murderer. The detective expends all his resources and energy on proving the innocence of the suspect. Meanwhile, the real murderer is still running around, causing more harm.
In 2000, Rita Charon founded the Program in Narrative Medicine at Columbia University. In a 2001 paper she published in the The Journal of the American Medical Association titled “Narrative Medicine: A Model for Empathy, Reflection, Profession, and Trust,” she explains her program’s pedagogical aims:
The effective practice of medicine requires narrative competence, that is the ability to acknowledge, absorb, interpret, and act on the stories and plights of others. . . . Adopting methods such as close reading of literature and reflective writing allows narrative medicine to examine and illuminate 4 of medicine’s central narrative situations: physician and patient, physician and self, physician and colleagues, and physicians and society.
Charon has a Ph.D. in English as well as an M.D. In person, she vibes more empathic New Age guru than academic or medical professional. She speaks as though frequently surprising herself with what she’s discovered through the act of articulation.
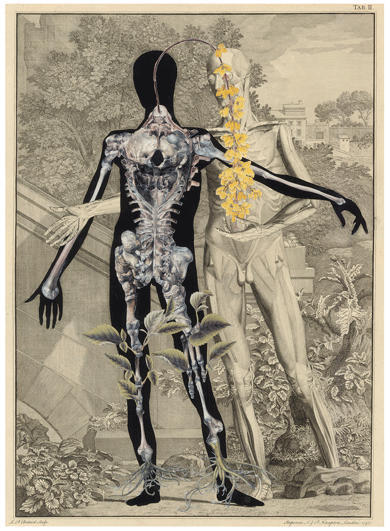
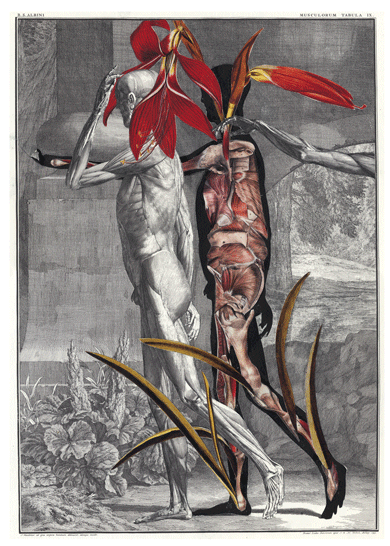
“The more I learned in a rigorous way how the novel worked,” she told me last year, “the better my doctoring became.” The act of close-reading a text — or studying a painting or a film — she maintains, equips students and full-time clinicians to become “better perceivers of multivalent scenarios.”
The narrative-medicine program has become a required part of the Columbia Medical School curriculum. Students must enroll in one of the program’s seminars — on literature, visual arts, philosophy, or creative writing — during the spring semester of their first year. Later, they can choose to concentrate in narrative and social medicine, pursuing a four- to nine-month “scholarly project.”
“We think there’s something to be learned from reports of lived experiences,” Charon says.
Charon cites her own clinical practice as a way to honor the subjective report. The usual entry point to doctor-patient interrogation is, “So what brings you here today?” or, “What medications are you currently taking?” Charon begins her patient interactions with what she calls “an invitation.” She says, “I need to know a great deal about your body, health, and life. Please tell me what you think I should know about your situation.”
The forty-four-year-old patient, female, continues to contend with her situation. She narrates it to anybody who will listen, because the more she talks about her inner-ear travails, the more information she gathers about other people who’ve suffered similarly. These stories could provide useful clues to identifying her own illness. For example. A friend in London’s girlfriend has ear-ringing that’s alleviated by osteopathic neck treatments and craniosacral massage. This same friend’s friend suffered from ringing, sound sensitivity, nausea, and dizziness and was helped by something called vestibular therapy. Her Midwestern cousin suggests that her crystals have been knocked out of place. She mentions her cousin’s crystal theory to a New York friend, who says, “That happened to me once.” This friend’s doctor performed the Epley maneuver, a gentle back-forth twisting of the head, which returned the delicate calcium crystals or “ear stones” to their proper location in the inner ear. A friend who lives in Maine without health insurance says that he, too, was often debilitatingly nauseated. His wife watched an Epley maneuver video on YouTube; she performed the move on her husband; his nausea disappeared.
At a dinner party the patient is introduced to another possible diagnosis. Her dining mate’s mother suffered from labyrinthitis. The symptoms match hers. Labyrinthitis, she learns online, can be caused by a virus. The patient remembers that she had a head cold before her ear problems started.
“Labyrinthitis,” her friends say, when she tells them of this possible diagnosis. “Of course you would get something called labyrinthitis.” This comment is a well-meaning joke about the patient’s penchant for writing labyrinthine novels. She does not disagree with the implication: stories in the head, she’s learned, can be expressed by the body. It’s a form of literary interpretation.
Peter Blake is a former executive producer and writer for the television medical drama House. Created by the Canadian writer David Shore, House was, according to Blake, “the first show to be devoted to one medical mystery per episode, in the same way that, say, Law & Order was devoted to one murder mystery per episode.” The problem, however, was that the “perp” is not a person but an ailment. “Viruses don’t have personalities,” Blake says. “They don’t have motives.” In a cop drama, the dramatic construction relies on carefully placed clues that prevent the viewer from accurately guessing who the killer is while also allowing the viewer, once the killer is revealed, to think, “Oh yeah, I should have gotten that!” No viewer of House thinks, “I should have known it was African trypanosomiasis!”
 Shore’s solution to these formulaic anomalies was to ground the show in the character of Gregory House, a rogue, Vicodin-addicted bully who mocks and emotionally abuses his patients (when he deigns to speak with them at all). Blake describes House as “amoral, a brain on legs, a doctor who doesn’t give a shit about people.” The question Shore wanted to pose to viewers: Would you rather have a doctor who held your hand and was a great listener or one who was an asshole but saved your life?
Shore’s solution to these formulaic anomalies was to ground the show in the character of Gregory House, a rogue, Vicodin-addicted bully who mocks and emotionally abuses his patients (when he deigns to speak with them at all). Blake describes House as “amoral, a brain on legs, a doctor who doesn’t give a shit about people.” The question Shore wanted to pose to viewers: Would you rather have a doctor who held your hand and was a great listener or one who was an asshole but saved your life?
This choice, of course, is rigged, as even House itself reveals. Unlike Emily Owens, the show doesn’t traffic in the stereotype (perpetuated by the attitudes of too many actual doctors, unfortunately) that doctors listen to patients at the expense of diagnostic objectivity and efficiency. House, while he professes not to care about humans and their personal stories, deeply, to his shame, does. What helps him crack each case is never a test or an algorithm; it’s a secret the patient has not told House’s team about his or her life. A story that’s remained, until House diagnoses her, untold.
I recently decided that I have a talent for medical diagnosis, at least within the context of a TV show or book. When reading Jerome Groopman’s How Doctors Think, I correctly diagnosed the patient under discussion, by the second page, with celiac disease. When reading chapter four of When Doctors Don’t Listen, I correctly guessed that a patient with weight problems, mild asthma, and trouble staying awake suffered from obstructive sleep apnea. The moment pregnant Sybil complained of swollen ankles on Downton Abbey, I knew she had preeclampsia.
These are carefully crafted acts of symptom disclosure, however, not real patient encounters. The dramatic pattern is designed to be perceived. I am a highly perceptive reader when it comes to identifying these types of dramatic patterns. As a writer, however, I’ve begun to wonder whether this talent is a debility. I’ve begun to feel bad for my characters; I’ve begun to think of them as patients to whom I may not have listened properly, and whom I may have sent down one of Wen and Kosowsky’s diagnostic pathways — but the wrong one. In medical terms, they might be seen as victims of premature-closure errors, defined as a doctor’s (or, in this case, a writer’s) early dismissal of still viable narrative possibilities.
A particular phrase haunts me when I write fiction now. It’s a line from A Wilderness of Error, Errol Morris’s book about the famed Jeffrey MacDonald case, in which MacDonald, a former Green Beret, was found guilty in 1979 of murdering his pregnant wife and their two daughters. Morris believes MacDonald was convicted not by evidence or due legal process but by the popular narratives at the time, especially those about psychopaths. These were propagated by such books as The Mask of Sanity, a work of non-fiction by the psychiatrist Hervey M. Cleckley. Cleckley’s psychopaths walked among us. They were monsters in disguise. People were hungry for more. A TV movie portraying MacDonald as a psychopath aired on NBC in 1984. This miniseries was based on Fatal Vision, the journalist Joe McGinniss’s true-crime account of MacDonald’s story and legal appeals. After the book’s publication, MacDonald sued McGinniss for fraud because McGinniss had pretended to believe in his innocence while at the same time writing a book portraying him as an inscrutable demon. These were just a few of the factors, according to Morris, that led to MacDonald’s conviction, and radically diminished his chances of a fair trial. He was, claims Morris, “condemned to the story that had been created around him.”
The female patient, still forty-four years old, makes an appointment with a highly recommended ear doctor. He has no openings for two months. In the meantime, she decides to see her GP.
When speaking to this doctor she can be a little wordier with her presentation. The doctor knows she is a fiction writer and is seemingly made happy by this fact. When she visits him, she experiences a self-imposed pressure to be a lively raconteur.
She tells the doctor about her symptoms. She is entertaining and engaging but hews to the salient facts. The doctor listens. The patient can sense when a person has made up his mind and stopped listening. He doesn’t do this. He waits until she’s finished talking. Then he thinks. Then he speaks. He says it sounds like she has labyrinthitis. That it takes a long time for the inner ear to recalibrate. That her symptoms should subside in a month or so.
The patient leaves feeling incredibly great. She’s still nauseated and her ear is still ringing, but it’s amazing how much less scared she feels just because someone listened to her.
Whether or not the GP’s diagnosis is correct, his prognosis comes to pass. Within three weeks, she is completely better. She decides to keep her appointment with the reputable ear doctor. Now she’s simply curious: What will he conclude from her story?
Rita Charon invited me to sit in on a class. She began by asking her students, all in their third year of medical school, to write for two minutes about an experience “of peril or protection.” Then she led a discussion about the novel the students had been assigned to read that week. They spoke ably about literary themes and patterns. They insightfully dismantled the book’s mechanics and mapped character motivations. The novel under discussion was, given my recent familiarity with certain terms, what I might now call a pathway novel. The patterns, while intricately woven, were easily recognized. There was complexity and symmetry to appreciate, but nothing that prompted differing opinions. A skeptical part of me wondered: Might reading certain kinds of novels actually reinforce doctors’ tendency toward overconfidence? Might it reinforce the belief that a patient is, like a character in some mainstream literature, a collection of traits that add up and “make sense” — the sort of sense that doesn’t require a second or third or fourth opinion? Might reading such novels make a person dangerously convinced (as I was, when I diagnosed Lady Sybil) that she is an unusually perceptive diagnostician and, moreover, that she is correct? How does reading this kind of novel not emphasize (rather than program against) pathway thinking? The curmudgeon-with-a-heart-of-gold pathway. The scrappy-immigrant-who-is-betrayed-at-every-turn-but-never-loses-his-faith-in-America pathway. Certain literature delights in part because of its reliance on familiar archetypes. The act of recognition makes you feel smart.
I asked the students whether they were capable of reading novels without medically diagnosing the characters: This unstable protagonist (were she to be examined by a professional), for example, would clearly earn a diagnosis of manic depression. This unemotional man would clearly land on the autism spectrum. This good-time Charlie would clearly qualify as an alcoholic.
The students assured me that they didn’t read books this way. But I do. I like to practice my diagnostic skills on old novels, in which the name of a character’s illness is often omitted. The author is not hiding the diagnosis from us; at the time there was no name for the illness. In Buddenbrooks, by Thomas Mann, the matriarch of the Buddenbrooks clan, Madame Antoinette, is beset by an illness that begins as a “slight intestinal catarrh” and progresses to “colic” and “vomiting spells.” She grows weaker and weaker. Two weeks later, she dies. What killed Madame Antoinette? Stomach cancer? Bacterial poisoning from meat left too long on the counter? A systemic strep infection that entered through a finger puncture she sustained while handling roses? I feel it is okay to wonder.
In 2011, the Association of American Medical Colleges concluded a three-year review of the Medical College Admission Test (MCAT), issuing a report with recommendations that, if followed, would “enrich the exam by giving attention to the concepts tomorrow’s doctors will need.” In addition to the usual hard science, the 2015 MCAT will include a “Critical Analysis and Reasoning Skills” section, which (presumably) tests for the exact comprehension abilities Charon is trying to identify and enhance. (The pre-overhaul MCAT, Charon told me, was useful only in predicting how well a student would do on exams once she got into med school.)
In April 2013, the New England Journal of Medicine published an article called “Reforming Premedical Education — Out with the Old, In with the New,” which suggested that most of the focus is (and has been, since the early 1900s) on undergraduates. Critics of the current model — which requires a student, before applying to study medicine, to spend her high school and college years studying premedicine — complain that technological advances have made the memorization of enormous amounts of information moot, that the rate of scientific discovery renders outdated much of the education a student receives, that the present system fails to cultivate “self-directed lifelong learners,” that the test-taking culture (itself now a major money industry) not only disadvantages women and minorities but spreads an affliction called premed syndrome — a cutthroat, grade-grubbing obsessiveness that, at best, produces the sorts of doctors who inspire laughably accurate stereotypes on TV medical dramas and, at worst, clashes perversely with one presumed goal of becoming a doctor in the first place: working together to help others. The NEJM offers this upbeat summary:
Various solutions have been proposed, but little substantive change has occurred. Universities are neither equipped nor motivated to create new courses for medical school preparation. They have limited resources, siloed departments, educational inertia, and faculty with ingrained teaching habits.
Peter Blake, when asked how the writing of House evolved over its eight seasons, observed, “at the beginning I’d start with a cool disease and try to figure out an interesting patient story to fit the disease. Then I started out with a cool patient story and then find a disease to fit. I started with the character, and then began laying in the medicine.”
Last summer I was sent a link to a Wall Street Journal article titled “A Better Online Diagnosis Before the Doctor Visit.” (The subhead: “As Internet Symptom-Checkers Improve, Health-Care Providers Say It’s OK to Search.”) The article spoke of previously held beliefs about the pitfalls of self-diagnosing on the Internet, then delivered the promised update:
Now more health-care providers are turning the tables, steering patients to new and improved computerized symptom-checkers that make it easier for them to get reliable information about possible diagnoses, research their condition and even connect directly to a doctor.
The article included a link to a symptom-checker called Isabel. I clicked on it. I entered my information: female, 40–49, North America, not pregnant. I input four symptoms I had been experiencing recently:
Ear ringing
Nausea
Ear pressure
Ear popping
Isabel generated a list of fourteen possible diagnoses sorted into common and uncommon, some affixed with a red flag, meaning immediate medical attention was recommended. Among my possible diagnoses were:
Ear Infection
Acoustic Neuroma
Meniere’s Disease
Sensorineural Hearing Loss
Ear Wax Impaction
Concussion
External Otitis
Acute Labyrinthitis
When I clicked on a diagnosis I was taken to a “Knowledge Window,” which consists of the relevant Wikipedia article bordered by a customized Isabel sidebar offering links to MedlinePlus and WebMD, among others. Some of these Wikipedia pages redirect (acoustic neuroma redirects to vestibular schwannoma).
The site is efficient; it undoubtedly saves a patient time if, like doctors, she is pressed for it. Back when I first experienced my symptoms, I probably would have appreciated both the shortcut and the reassurance: I was searching in officially sanctioned medical territory.
But after the hours of “online learning” I’d dedicated to my illness — following this patient thread, cross-checking my symptoms versus this other person’s symptoms, eliminating this diagnosis but opening up the possibility of another — I experienced the Isabel approach as blunt, overwhelming, and all too familiar. Isabel teaches patients to approach and understand their bodies the way the doctors they’ll eventually see will likely approach and understand them. It teaches patients to think algorithmically. It teaches them to look for clear answers instead of encouraging them to think more broadly about their condition. I didn’t recognize, for example, that a tight jaw was a possibly relevant symptom until I stumbled, after days of searching, upon a patient diagnosed with TMJ whose inner-ear symptoms matched mine.
Isabel, at this early phase, was also absent the experiences of other humans (the site has since added a “Patient Stories” feature, but at the time of writing there were only two featured — one about necrotizing fasciitis, another about unusual behavior in a five-year-old), which is what I find makes the Web such an unprecedentedly useful — if time-consuming — patient tool. Patient forums make the aims of your searching start to shift. You stop obsessing over a diagnosis — none really seem to fit perfectly, after all — and instead start focusing on symptom relief. Other people have suffered these same symptoms; how did they alleviate or cure them? The goal, you might realize, is not to name your condition. The goal is to feel better.
Christopher Illick, a gastroenterologist and assistant clinical professor at Yale School of Medicine, observes that the med-school admissions process — with its emphasis on test scores and grades — privileges “black-and-white” thinkers, as does the general curriculum.
“You do not learn gray-area thinking,” he told me. “Not at all.”
Illick taught the following clinical procedure in his physical-diagnosis class: He told his students that they should allow the patient five minutes to speak and that they should ask only open-ended questions during this period. After the five minutes are up, the doctor can ask more pointed questions, start to rule things out, and approach a diagnosis. Illick says he strives to “teach students how to listen” and that “there’s one answer to an equation, but many ways to hear a story.” He also says, of this clinical approach, “If you let someone speak, they may not take you to the diagnosis. But they’ll definitely take you to what they care about.”
Illick cites as the most promising sign of medical-education reform the Mount Sinai Icahn School of Medicine’s “early assurance” program. Begun in 1987, this program allows interested students to apply and be accepted after their freshman year of college. Illick, himself a “liberal artist” — his half-joking term for a doctor who did not follow the premed track — also works as an adviser to Yale undergraduates. He mentions one of his freshmen from four years ago. This student was at Yale to play basketball; training and travel meant he wasn’t able to take many of the required premed courses. He applied early assurance at Mount Sinai and was accepted; meanwhile, he was able, during the rest of his undergraduate career, to compete as an athlete and pursue his other field of interest, art history. Instead of dedicating those years to learning information he’d relearn or no longer need, this student was, in Illick’s words, “teaching his brain to be human.”
Illick was being neither hyperbolic nor ironic. To the weary, if still idealistic, the culture of medicine might seem to force this choice on its practitioners — doctor or human? This binary is so institutionally entrenched that it is practically, but not actually, fodder for puns. The official name of Mount Sinai’s early-assurance program, no playfulness (I think) intended, is HuMed.
Here are Isabel’s proposed diagnoses for Madame Antoinette Buddenbrook (female, 50–64, Western Europe, not pregnant): heavy-metal intoxication, CVA/stroke, gastric volvulus, botulism, polyneuropathy disorders, myasthenia gravis, upper-urinary-tract obstruction, acute porphyria.
Only CVA/stroke and acute porphyria have red flags attached (I’m assuming Madame Antoinette, given that she died, might have benefited from semi-quick medical attention). When I click on the CVA/stroke link, I am taken to the Wikipedia landing page for errant searchers: “Wikipedia does not have an article with this exact name.”
In her book Why Do We Care About Literary Characters?, the Stanford English professor Blakey Vermeule writes, “Caring about anybody takes energy, and when we care about fictional people, the costs seem unlikely ever to be recouped. Why should we spend attention on people who will never care about us in return?”
In the medical realm, caring — possibly to the point of knowing a patient the way a village healer might — requires time that most doctors cannot afford to spend. Those costs, so the common thinking has been, will never be recouped. (Patients are not the only victims of this thinking. A recent New York Times blog post titled “Who Will Heal the Doctors?” suggests that physicians are equally disillusioned with their profession and the productivity model that drives it.) But research shows that the more caring and compassionate the doctor, the better the health outcomes, and the lower the ultimate costs of treatment. According to an article that appeared last year in Becker’s Hospital Review, “Healthcare Emotional Intelligence: Its Role in Patient Outcomes and Organizational Success,” higher degrees of empathy correlate with fewer medical errors and improved overall satisfaction for doctors, nurses, and patients.
But patients’ desire for less invasive (and often less expensive) treatment is still being ignored. In a recent paper in the New England Journal of Medicine (“Shared Decision Making to Improve Care and Reduce Costs”), authors Emily Oshima Lee and Ezekiel J. Emanuel cite a study in which “only 41 percent of Medicare patients believed that their treatment reflected their preference for palliative care over more aggressive interventions.” As Lee and Emanuel point out, treatments for preference-sensitive conditions (such as prostate cancer and hip arthritis, which do not have clear courses of treatment) should vary widely, just as patients’ individual circumstances and values do. Yet most of the variation exists not between patients but between hospitals; the data indicate that doctors, not patients, are making the decisions, and they are doing so on the basis of financial incentives.
One possible reform might be found in what Lee and Emanuel’s paper refers to as a “sleeper provision” in Section 3506 of the Affordable Care Act. The “program to facilitate shared decision making” would seek to develop “patient decision aids” in the form of written materials, videos, and computer presentations. Once standardized, the aids would be a required step in clinical protocol for all doctors treating patients with preference-sensitive conditions. Among other suggestions, Lee and Emanuel recommend that the program, which has yet to be funded, be enforced through the implementation of financial penalties. Doctors who do not share and discuss the decision aids with their patients would not be fully reimbursed by Medicaid or Medicare for their services.
That such oversight is necessary should probably strike us as more absurd than it does. We must offer humans who have self-selected to dedicate their lives to helping other humans special incentives to listen to the desires of those humans. We must ensure it is financially advantageous for doctors to communicate with, and ideally not fleece or endanger, their patients. Such a system can make seemingly radical reactions to medical overtreatment appear actually quite reasonable. The most common operation among American women — the C-section — has helped spawn an active resistance movement: home birth. This movement arose in response to the intervention- and profit-heavy culture that has come to define the U.S. hospital birth. Home birth might in the future be seen as the harbinger of a patient revolution: if patients continue to be restrained from actively participating in their own diagnosis and care (and in a way unmotivated by cost creation), patients, whenever possible, will stop going to doctors. The contentious nature of the home-birth movement also points to the reality that patient-doctor collaboration is, at the moment, often nonexistent. Given the lack of any friendly middle ground, patients adopt extreme attitudes: If we cannot collaborate on this project, my body, then forget it.
Before she visits the highly recommended ear doctor, the patient researches the bladder condition it turned out she didn’t have: interstitial cystitis. Interstitial cystitis is identified through a process known as diagnosis by exclusion. There is no reliable test to prove a patient has interstitial cystitis; a doctor can only rule out every other possible illness or disease that produces similar symptoms.
For the month that the patient believed she had interstitial cystitis, she had a complicated relationship to her diagnosis. She found that she did not want to accept it as hers. The reason was no mystery. According to a 1998 survey cited on Wikipedia, 40 percent of IC sufferers cannot go to work, 27 percent suffer “marriage breakdown,” and 55 percent contemplate suicide.
 But she also felt comforted that there existed a name for her suffering. Her pain was officially recognized by medical experts, who thus took her problem seriously. Until recently, this would not have been the case. Like many diseases in women characterized by pelvic pain, IC was thought for many years to be a psychosomatic manifestation of hysteria, brought on, it was sometimes thought, by episodes of childhood physical or sexual abuse. Not until 1987 did the National Institutes of Health convene workshops to establish the criteria for definition and diagnosis of the illness, and it was 2002 before the Social Security Administration acknowledged IC as a “severe impairment” and an official disability in the United States. Such recognition means a doctor won’t tell a patient, “It’s all in your head.” These would seem to count as unqualified improvements in care.
But she also felt comforted that there existed a name for her suffering. Her pain was officially recognized by medical experts, who thus took her problem seriously. Until recently, this would not have been the case. Like many diseases in women characterized by pelvic pain, IC was thought for many years to be a psychosomatic manifestation of hysteria, brought on, it was sometimes thought, by episodes of childhood physical or sexual abuse. Not until 1987 did the National Institutes of Health convene workshops to establish the criteria for definition and diagnosis of the illness, and it was 2002 before the Social Security Administration acknowledged IC as a “severe impairment” and an official disability in the United States. Such recognition means a doctor won’t tell a patient, “It’s all in your head.” These would seem to count as unqualified improvements in care.
However: Now that her disease had a name, it also had a narrative. When a patient is told by a urologist that she has IC, she will also be told that there is no cure and no treatment and no reliable way to stop the pain. Some doctors prescribe Elmiron, the only drug approved by the FDA to treat IC, or off-label uses of Neurontin, an antiseizure medication, and various SSRIs; others prescribe TENS (transcutaneous electrical nerve stimulation); in severe cases, patients undergo a bladder wash with a dimethyl sulfoxide solution.
The patient decides not to take drugs or subject herself to invasive bladder procedures, not yet. Instead she visits a pelvic-floor physical therapist, offhandedly mentioned by her urologist as a possible means to “manage her pain baseline.” Not to mince words, this therapist puts her gloved hand into the patient’s vagina and examines her pelvic-floor muscles. (Her urologist, a very attentive listener, has never once touched her.)
The patient, the therapist reports, has a spasming pelvic-floor muscle.
The patient asks, “Does this mean I don’t have IC?”
The therapist says, “IC is extremely rare, and in my opinion really overdiagnosed.”
She then admits that many pelvic-floor physical therapists don’t believe that IC exists. To clarify: these skeptical therapists believe that the symptoms exist, but they do not endorse the name given to these symptoms by doctors. They reject it because of the narrative that clicks into gear once the name “IC” is appended to a patient.
Pelvic-floor physical therapists use an umbrella term — pelvic-floor dysfunction — and this more flexible term has a wider variety of prognoses and treatments. Once the patient has been given this new name for her symptoms, her story is completely rewritten. Her pain — formerly deemed chronic and incurable — after a number of therapy sessions over a period of months, disappears.
In the aftermath of this experience, the patient thinks about naming. How naming is a useful way for doctors to identify and define a collection of symptoms that prove otherwise a puzzle to them. To name this befuddling collection is to reassure their patients, whom they desperately want to calm and help, that they at the very least can say what is wrong with them, even if they can’t offer a cure. To name a collection of symptoms is to give the patient what she believed, until recently, she most wanted when she went to a doctor: a firm diagnosis.
Despite his caustic (and entertainingly intemperate) rendering, Dr. Gregory House — the “brain on legs” — reminds us that the human brain is not, by anatomical rights, a humanizer. Yet there persists a fear that the use of computers in the medical sphere is the mark of an increasingly dehumanized system. While I have been dehumanized by quite a few overworked and time-challenged doctors, I have never been dehumanized by my computer. My computer — in collaboration with me — works tirelessly on my behalf. It is always there to take another question. It is not offended when I doubt its findings.
There are those who argue that the computer is, in fact, an essential component of a more humane and patient-centered medical practice. That doctors could use computers not as an excuse to spend less time with patients but as a means to spend better and more focused time with them.
The computer’s role in the future of health care has also been embraced by village-healer advocate Dr. Oz. In July 2012, Oz’s interactive health-and-wellness social network, Sharecare, bought Problem Knowledge Coupler Corporation (PKC), a company founded in 1991 by the physician and professor Lawrence Weed. Weed, co-author of a book called Medicine in Denial, has long criticized med schools for “giv[ing] students a misplaced faith in the completeness and accuracy of their own personal store of medical knowledge and the efficacy of their intellects.” Weed is also frustrated by the fact that schools teach students to find a single diagnostic solution when most patients present the interaction of multiple diagnoses or disorders. To help develop “a medical care system in which patients are no longer dependent on the limited, personal knowledge their caregivers happen to possess,” Weed created Problem-Knowledge Coupler, a software program that supplements a single patient’s medical record with an analysis of all the available and related medical data (including other patient records), then generates a “readable narrative form” that presents a range of diagnostic possibilities for the doctor and patient to consider.
Given the amount of available medical data, the village healer — the health-care authority who knows all there is to know, yet also has the time to deeply acquaint him- or herself with every patient — cannot exist nowadays without computer assistance.
Computer-based clinical reforms are in the service of human encounters. Patient-centeredness, while it may sound passive — the patient as the sun around which medical and paramedical professionals orbit — in fact requires the patient to be a highly active co-detective. It also requires that she relinquish the need for the kind of clear answer she’s come to expect when she goes to a doctor’s appointment.
But a confident diagnosis — and a godly doctor unto whom we can helplessly deliver our malfunctioning bodies — is so very hard to give up. Though I know better, I still go to doctors desperately believing in their authority and wanting a recognized name for my illness; I want the uncertainty corralled and explained, I want my future narrative to be predictable based on a time-tested treatment for my recognized problem and to require no agency on my part. But bodies don’t work that way. Doctors shouldn’t be expected to work that way, either. Patients need to be re-educated, too.
In the meantime, how might patient agency and acts of collaborative diagnosis start to emerge in clinical practice, despite the hopeless, intractable educational system described by the NEJM? The Internet isn’t going away, so how can doctors — those who aren’t, like Kyle Putnam on Emily Owens, M.D., busy developing a medical pidgin — adapt to and even capitalize on its presence? It might start with doctors acknowledging, and learning to use to their diagnostic advantage, the increasingly informed patient base. A patient’s Internet findings or conclusions, even if wrong, are not irrelevant information. How a person understands her symptoms, and what prevailing symptom inspired the Internet search, could tell the doctor quite a bit. This is how the patient articulated her suffering to herself; this is how she first put it into words, before she had to form actual sentences and tell her beginning-middle-end story to another person. I can imagine a time in the near future when the doctor says not, “So what’s bothering you today?” but rather, “Tell me about your search terms.”
The patient, forty-four years old and female, finally attends her appointment with the highly recommended ear doctor, male. Not a listener, either, this ear doctor. Brusque and in a hurry. It doesn’t matter, however, since the patient is totally asymptomatic now. The stakes are low.
She tells her story again. She omits her visit to her GP and his diagnosis, but she does mention the first ear doctor and the Ménière’s diagnosis. The doctor says, “This doesn’t sound like Ménière’s.”
After listening (sort of) to the patient’s symptoms, of which she stresses the nausea was the worst and most debilitating of all, the ear doctor proclaims that the patient has a TMJ issue. The patient is secretly delighted by this diagnosis. This means she wasn’t totally off-base when she researched her symptoms months ago and discovered TMJ to be one possible explanation.
She asks the doctor what one does to treat TMJ, though of course she already knows the answer to this question. The doctor recommends a mouth guard worn at night, and ibuprofen for the neck and jaw soreness. “What about physical therapy?” the patient asks. She has read countless articles about TMJ physical therapy; TMJ specialists swear by it, as do patients.
“I don’t usually send TMJ patients to physical therapy,” the doctor says. “Physical therapy doesn’t really help. Just get a mouth guard. And take ibuprofen.”
She considers pulling up on her phone the many expert opinions — issued by doctors every bit as reputable as this one — that contradict this doctor’s belief about physical therapy.
Instead the patient puts on her coat. Then she remembers her most debilitating symptom. The nausea.
She asks the doctor, “So does TMJ explain the nausea?”
“No,” the doctor says. “TMJ doesn’t cause nausea.”
“But that was the most debilitating of my symptoms,” says the patient.
The doctor doesn’t respond.
“Is it possible,” the patient says, thinking of her GP and his diagnosis, “that I had labyrinthitis, and also a persistent if mild case of TMJ? Is it possible that my symptoms were caused by two simultaneously occurring problems?”
“It’s possible,” says the doctor.
The patient senses the doctor getting miffed.
“Well,” she says, trying to leaven the tone, “thank you for telling me I don’t have Ménière’s disease! That never sounded like the right diagnosis to me.”
The doctor takes a moment. Then he responds, not unsarcastically, “I’m glad I could give you the diagnosis you wanted.”
The patient leaves. She feels angry and condescended to, but why? The truth is, he did give her the diagnosis she wanted.
But a diagnosis is not what she really wanted. What she really wanted was reassurance that her future visits to doctors won’t always involve an act of deceit, won’t require her to pretend she doesn’t know anything about her own condition, or to feign respect for a doctor’s supposed expertise while silently knowing that there are many other doctor and patient testimonies that contradict or complicate his or her opinions. Even though she and the doctor presumably want the same thing — to return her to a state of health — she cannot ask this far-better-educated doctor to help her parse and process the information that it’s her obligation as a “connected” human in 2014 to know and consider.
The patient is enraged and feels something akin to despair. If she’s honest with herself, what she wanted from this appointment was not in the doctor’s power to give her. She wanted to be cured of what she has come to know and cannot ever seem to fully forget: her body will fail her. Health, from the sober position she currently occupies, appears even more fickle and capricious than the illnesses that recently befell her. “Those who are not sick now will be sick anon,” Rita Charon said at a reading of Virginia Woolf’s essay “On Being Ill” that the patient recently attended. The patient considers the possibility that she’s mistaken what is essentially her midlife crisis for a wholesale failure of the medical system. She has not been uniquely misunderstood by any human being other than herself. What she’s interpreted as the shocking fallibility of her doctors is more accurately interpreted as a normal rite of passage — her move from the world of health into the world of unfixable ailments and, eventually, her demise. No doctor will be able to prevent death from happening to her.
She is reminded, not for the first time during this process, of her former and beloved GP, the one she saw until she was thirty-eight. He always had time; he always listened. He was self-doubting and open to new information. Whatever went wrong with her body, she knew she had a sensible and kindly collaborator. He was killed in 2006 while riding his bike on the West Side Highway bike path in Midtown Manhattan. A city tow truck hit him. When he died, she castigated herself that she’d told him so much about her body yet she’d never told him how she felt. She’d never told him how important he was to her, what a savior he was, even on the days when she was healthy. She enjoyed her health more knowing, should she lose it, that he’d be there to help her. His name was Carl Henry Nacht.
She recalls a question she was asked by the very first ear doctor, the one who thought she might have Ménière’s. The doctor was curious about the ringing. She said, “Before the ringing started, what did it use to sound like in your ear?”
The patient had tried to remember what it used to sound like in her ear before the ringing started. She couldn’t. Now the irony of this failure strikes her. She should try to hear what she’s previously ignored. She should try to register what the absence of illness sounds like while she’s lucky enough to be able to appreciate all that’s not there. She stops on the sidewalk. She closes her eyes. She listens.