It was a miserable January morning in Marion, Alabama, last year, with temperatures twenty degrees below average and freezing rain that sliced sideways. But that did not dissuade the people lining up outside the Perry County Health Department. The first appeared at the door when the sun had barely risen, then a couple more arrived, and soon they came by the hundreds. Some brought their children, others showed up with cousins; there were families four generations deep. By nine o’clock, the line had lassoed around the building, with its tail pitching into the parking lot. People held umbrellas in one hand and with the other gripped handkerchiefs or scarves tightly across their mouths. Many were from the same neighborhood, and most were black. All of them had come to collect twenty dollars in exchange for getting tested for tuberculosis.
Shane Lee, Marion’s town doctor for the past quarter-century, pulled his taupe pickup truck into the parking lot. His clinic was kitty-corner to the health department, and he was having trouble finding a spot. It was Lee who had discovered the community’s first severe case of TB, a little more than a year earlier. In October 2014, a nurse practitioner tore into his office with a fresh medical mask over her mouth, frantically waving an X-ray film. The mask, a tight-fitting turquoise respirator, was unusual. And then he looked at the radiography, which showed that the patient’s lungs were nearly completely whited out. It was the worst case of tuberculosis that he had ever seen.
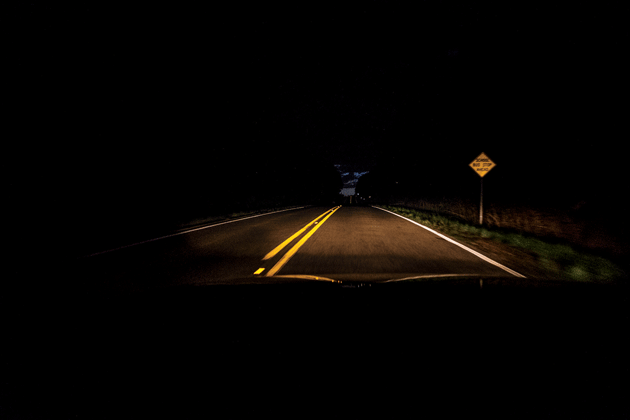
The road from Marion to Greensboro, Alabama, the site of the closest hospital. All photographs by Nina Robinson
Since then, Marion, a town of 3,500 and the seat of Perry County, has been grappling with a historic outbreak of a disease that has vanished from worry in much of the United States. Thirty-four active cases have been found; if that doesn’t seem like a lot, consider that the rate of infection — what the World Health Organization uses to determine severity — is almost a hundred times the national average, and higher than the rates in India, Kenya, and Haiti. Nearly 200 more in Marion were discovered to have latent tuberculosis, meaning that they were infected but had not developed active symptoms — which include bloody coughing, shortness of breath, night sweats, and weight loss.
There is no hospital in town. The nearest one, twenty minutes away in Greensboro, has minimal resources. The road to get there is narrow, unlit at night, and littered with roadkill. Perry County has only two ambulances, one of which is on standby for the local nursing home. Life expectancy here is seven years lower than the U.S. average, and the percentage of obese adults is almost a third higher; by the latest count, more than a quarter of births take place without adequate prenatal care. Lee’s clinic is Marion’s only place for X-rays.
When he saw the image of the infected lungs, he called Pam Barrett, the tuberculosis controller for the state of Alabama, in Montgomery. She conferred with her team, and as Lee alerted them to signs of infection in more patients, they realized that all the cases originated from the same place — an impoverished African-American neighborhood called the Hill. While encounters at the grocery store or the hair salon can, on rare occasions, transmit TB through the air, repeated and extended exposure — living in the same apartment, for instance — puts someone at the greatest risk. This was how the disease was spreading in Marion. “We knew all the cases were coming from the Hill,” Barrett told me recently. “Nobody else needed to be tested unless they were close contacts.”
The case Lee saw in that first X-ray was at an advanced stage, and the patient died. Though the health department’s staff tried to track those who might be vulnerable to infection — they traced the patient’s immediate contacts until they found someone positive, then traced that person’s contacts, working outward — most people declined to speak about others in their midst, even when they came for screenings at Lee’s clinic.
If the team wanted any chance of containing the outbreak, they needed to connect with the Hill’s residents quickly. Barrett came up with an idea: a health fair to test them, an event planned not as “a tuberculosis thing” but as a fun community gathering with free pizza and soda, token giveaways, and raffles for cash. In addition to TB screenings, the fair would offer blood pressure monitoring, finger pricks to check glucose levels, nutrition counseling, and sexual-health education materials. To get local buy-in, her staff partnered with Sowing Seeds of Hope, a Christian community-development organization in Marion, which loaned its logo for flyers and helped post them around town. While location scouting, Barrett personally passed word on to the guys who frequented the Hill’s basketball court.
Early one Saturday morning that November, Barrett and her colleagues drove several hours from Montgomery to the Hill. They convened at the basketball court and began setting up tables and supplies. But shortly after they got started, a group of young men appeared and threw beer bottles at them, which whipped past their heads and crashed near their feet. The health workers ducked for cover. The men shouted expletives, then ran off. Barrett called the police. Soon, two sheriffs stationed their car conspicuously out front. Eventually the testing began, and the health workers kept on until the afternoon. But turnout was low, and no active cases of TB were found.
“I’ve done health fairs all over this community, and I’ve never had that kind of reception,” Frances Ford, a native of Marion and the director of Sowing Seeds of Hope, told me. The health department ran into trouble, she said, by popping in as outsiders and declaring their intention to concentrate solely on this neighborhood. Barrett, unlike the people she was trying to reach, is white, and though some members of her team are black, they didn’t know the town. “They targeted African-American people — they referred to them as ‘the people on the Hill,’ ” Ford explained. “The way things were said, the wording. It was stereotyping. That’s what I heard.”
Over the next year, the outbreak continued to rage. Desperate, Barrett decided to try something that the health department had never done before: a cash reward. Twenty dollars to get tested; twenty more if patients returned to pick up their results. If those results were positive and patients followed up for chest X-rays, another twenty would be disbursed.
On that January morning in 2016, as the financial-incentives program began, Barrett’s team finally made some headway. One by one, people from the line around the health department were let in, and during the next three weeks, the state’s nurses and doctors managed to test more than 2,500 people. All told, the project cost the state of Alabama $235,000.

Shane Lee on his way to a house call
“No public health department has money lying around to pay people to look after their health,” Richard Chaisson, the director of the Johns Hopkins Center for Tuberculosis Research, told me. I asked the health workers why they didn’t consider simply going door-to-door around the Hill instead. It would have been less expensive, more personal, and easier to trace members of a household. One of the nurses, a white woman, replied: “If we wanted to get shot.”
Ford was aware that the Hill had a reputation for being dangerous, but she wanted me to know that she didn’t share this view. “I’ve never seen anything that I feel uncomfortable around,” she said.
When a disease outbreak occurs, Chaisson explained, “the norm is panic, for people to demand testing from the health department, and you can’t do it fast enough.” But the Hill has never been much for demands. The town of Marion sits in the belly of the Black Belt — historically, a ribbon of seventeen counties in central Alabama and parts of northeastern Mississippi, where whites enslaved black people to farm cotton in the dark, fertile soil; the term has come to refer broadly to predominantly African-American areas in the rural South. Across the Black Belt, there is grave poverty; Alabama is the fourth-most-impoverished state in the nation, and Perry is its worst-off county — 47 percent of residents live below the poverty line. The burden is shouldered unequally, as the poverty rate in Perry County is three times higher for black people than for whites. Jim Crow is gone, yet segregation lingers, along with its associated injustices. While Black Belt districts typically go blue, the rest of their states are deep red; last year, after the state of Alabama enacted a law requiring photo identification to vote and then promptly closed D.M.V. offices in Black Belt counties, a federal investigation confirmed that this targeting amounted to discrimination.

Lee’s clinic, near downtown Marion
History feels present in this part of the country, and the past has provided good reason for people to be wary of the medical establishment. In 1932, the Tuskegee Study of Untreated Syphilis in the Negro Male was conducted only two hours away from Marion. Scientists rounded up a group of uneducated sharecroppers, many of whom had syphilis, for long-term research. In the 1940s, when penicillin proved curative, the researchers left the group untreated; many subjects suffered severe complications of syphilis and infected their partners and children. Lee told me that during the health department’s tuberculosis campaign, his nurse saw a Facebook post circulating among people in town that compared the testing to the Tuskegee study.
There are similar stories throughout the Black Belt. Beginning in the 1920s, doctors performed hysterectomies and tubal ligations on black women without their consent; this practice, the “Mississippi appendectomy,” continued for decades. In 1933, North Carolina assembled a five-person eugenics board, which included physicians, that launched a sterilization campaign of “unfit individuals” — mostly poor African Americans — for the sake of their “best interest and welfare.” The program wasn’t dismantled until the late 1970s.
In 2010, after the Affordable Care Act went into effect, Alabama chose not to expand Medicaid. Governor Robert Bentley, a doctor who recently resigned following reports that he used state funds on an extramarital affair with an aide (the one who proposed the D.M.V. closings), argued that it would cost too much and make “able-bodied individuals” dependent. “We will not expand on a flawed and broken system that encourages greater reliance, not on self, but on government,” he said, declining federal dollars that would have extended health insurance coverage to anyone earning less than $16,394 a year. In Perry County, where the average income is just under $15,000 and about 20 percent of residents are uninsured, that expansion would have been transformative.
When Donald Trump entered the presidency, Republicans proposed a replacement plan that threatened to make matters worse: the American Health Care Act, which took aim at Medicaid, out-of-pocket cost assistance, and tax credits. It also required people who lacked coverage for more than two months to pay a 30 percent surcharge when they finally bought it again — an especially burdensome policy in Marion, where employment frequently comes and goes. The bill failed to garner adequate support in Congress and many members of the G.O.P. backed off. But Trump has said that he expects to see a new deal by next year, and the far-right-leaning Freedom Caucus has clung to its mission of dismantling the A.C.A.
That prospect looms darkly over Perry County. When I asked Frances Ford about coverage, she told me, “It’s an impossibility for people. And these people are trying to work. Some people here are going to say it’s not worth working.” She went on, “You’re working, and all your money is going to health insurance.”
Several months after the state’s paid testing, I drove into Marion. I passed a residential area with beautifully restored antebellum mansions, and the town’s courthouse, a gracious building with magnificent columns. But as I wandered around the commercial strip of Washington Street, which runs two miles between the health department and the Hill, the sights revealed themselves gloomily. The door of a red building on a corner had years ago opened to the Ole Theater Cafe. There had been a clothing store, a stationery store, an auto-body shop, a restaurant or two. Now their storefronts were closed and battered-looking.
When I reached the Hill, I turned left at a weather-beaten used cars sign, parked, and made my way toward the site of the health department’s ill-fated fair. An old Buick was parked there; four men sat inside drinking beers and bobbing their heads to Michael Jackson’s “Black or White.” I went up to the window. The man sitting in the front passenger seat kept his hand firmly planted on a rifle resting against his left thigh.

Left: The Hill neighborhood. Center: Washington Street in downtown Marion. Right: The Hill’s basketball court
I was there, I said, to see Orlando Moore, who lived in the neighborhood. We’d met before, and had made arrangements to discuss the TB testing. The man wasn’t sure where Moore was, but eventually I spotted him — a short, scrawny guy with a fade and a gold hoop in his left ear — sitting in a white car nearby. Moore, who was thirty-one, used to drive a truck and mow lawns. Now he had no job, and was expecting his first child — a boy — with his girlfriend, Charnissa, who was in the driver’s seat. He nodded as I approached the window. “Hey, you found me,” he said. There was a woman in the back, who introduced herself as his cousin.
Moore invited me over to his apartment. In the kitchen, he pulled a bottle of juice from the refrigerator and sat down. The women hovered around us, quiet at first. I asked about the testing. “The Hill’s used to being targeted,” he said. “Have you ever had to deal with white people? They look at us as one of the lowest families in Marion.” The Moores had been there for generations. He told me that he got tested when the health department offered a cash reward, but added quickly that the results were negative and that he didn’t know anyone who had the disease. His cousin, wearing a rainbow-striped dress, chimed in to agree.
Charnissa was incensed over the way the health workers had zeroed in on their neighborhood. “They’re singling us out,” she said, her voice rising. “Just because we’re around! Nobody here had it!” Exasperated, she stormed outside.
I took that as my cue to go. As I headed off, I bumped into Marsha White, a middle-aged woman in a pink-and-white summer dress and knee-high boots, sitting on a kitchen chair outside her apartment. I asked her about the outbreak, and she told me candidly that she had been diagnosed with TB and had gone through treatment. “I’m not ashamed of it,” she said, which she acknowledged was unusual on the Hill. She’d discovered that she was infected when her sister pointed out that she appeared to have lost a lot of weight. “I took all my clothes off, looked in the mirror, and I started crying,” she recalled. “And every time I walked or talked, I got short of breath.” She was a patient in Lee’s clinic, and she praised the health department workers for looking after her. Without them, she said, “I think I would’ve died.”
We talked for a while, and after a few minutes, Moore’s car appeared on the block. He and Charnissa half-waved at me. His cousin jumped out of the back seat and greeted White with a kiss on the cheek, grabbing some cigarettes from her pocket before dashing off again. “That’s my baby girl,” White explained.
I hadn’t realized that they were family. Lowering my voice to a whisper, I asked if she had kept her TB diagnosis from her daughter.
She chuckled and slapped her thigh. “My daughter? She knew I had it! Her boyfriend also had it!”
I was confused — I told her that, moments earlier, they’d all said that they were healthy, and so was everyone they knew.
“Them folk don’t want you to know what’s going on with them,” she said. “She just told you a lie.”
The apprehension I encountered in Marion was so well founded that I wondered if any outsider could surmount it. “I think they trust me as a person,” Shane Lee told me. “Because I’ve been here forever. But there’s an inherent distrust of the system in general by the black community.”
At fifty-five, Lee — a “blue-collar doctor,” as he called himself — had the build of a former football player, with light, ruddy skin and a sandy-brown mustache. He was serious and a bit gruff, reserving his dimpled smiles for the very old and the very young. When I met him at his clinic, he greeted me with a brisk “Good morning, ma’am,” and brought me over to his truck to set off for the homes of patients who were too ill or immobile to travel. He usually did this once a week, on Thursdays. With his radio station tuned to Fox News, we rumbled along Washington Street up to the Hill. Hannah Zahedi, a second-year medical student who was shadowing him, rode with us.
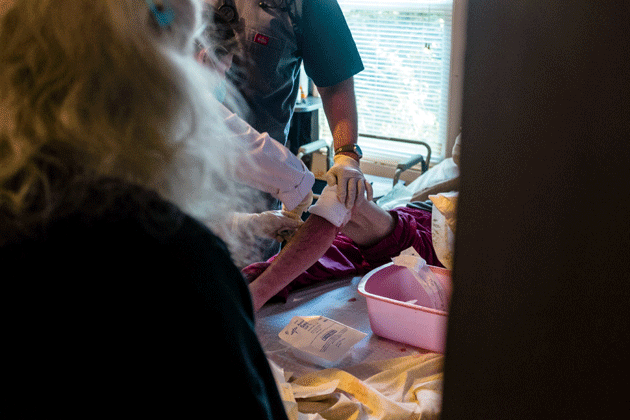
Lee treating patients during house calls
Lee is originally from Hueytown, near Birmingham. He’s a major general in the Army Reserve, a flight surgeon; for his family medicine residency, he trained not far from Marion, and started seeing patients here when the reigning town doctor made moves to leave. “I was recruited by the town banker and the pharmacist,” Lee said. “The town banker took me quail hunting. I like to hunt and fish and shoot ducks.” He and his wife settled on a 600-acre farm a few miles from the clinic. “This morning, as I drank my coffee, I saw two bald eagles,” he told me. “You don’t get that in the city, do you?”
We passed by Marion’s nursing home, where Lee serves as director. The building had housed a hospital until the late Nineties, when it could no longer pay its bills; the county remained more than $1 million in debt since the closure. Lee had been on its board. “Yeah, somebody’s going to have a heart attack at three a.m., but you can’t run a multimillion-dollar facility for one person having a heart attack at three a.m. every now and then,” he said. “That’s when you need good ambulance service and nine-one-one.” Since 2000, eighteen additional hospitals in Alabama have been shuttered, many of them in rural areas. Lee said that he and some Perry County officials would like to make emergency services more reliable, but there is never enough money in the budget.
Approaching another street, Lee pointed to a redbrick house that had been the home of Spencer Hogue, one of the original three people targeted in 1984 by Jeff Sessions — then the U.S. attorney for southern Alabama — for voter fraud. Hogue had been a patient of Lee’s, and he was diagnosed with latent tuberculosis before he died from other health problems, in September. “He was a no-kidding civil rights warrior,” Lee said.
Turning off Washington, we stopped in front of a one-story clapboard house. Thick weeds had overtaken the front lawn. Lee rapped on the door and roared, “Dr. Lee here!” We entered, following a woman’s voice to a room in the back, where she was mostly confined to bed because of polio. On her nightstand was a toothbrush, a tube of hand cream, and a bottle of hot sauce. Lee had already tested her for tuberculosis, and she was negative, but he continued to check up on her frequently. That morning, he wanted to confirm that she had gotten her annual flu and pneumonia vaccines.
“No colds in three or four years,” she said proudly.
On rounds, Lee doesn’t consult his phone or a notebook, and he knows the social situations of his patients as well as their ailments. He asked how she planned to get by now that her nephew, who had come from up north to help her for a few months, had returned home. “Oh, I’ll make do,” she said.

Lee treating patients during house calls
Lee seemed unconvinced. As we made our way out, he remarked, “It looks like you need new crutches.” He thought for a minute, then said, “I’ve got mine left over from my knee surgery. I’ll have Hannah here run back down and drop them off in the next couple of days.”
Then we drove off — Lee and Zahedi were seeing more than half a dozen patients before lunchtime. “He’s the only doctor I’ve ever been with that actually does home visits,” Zahedi told me. “It’s pretty cool. You never know who a patient is until you see them in their own environment. It really helps to see how they live.”
Zahedi, I learned, had family roots in Perry County. She was accompanying Lee as part of the Rural Health Leaders Pipeline, a medical education program that aims to build patient-doctor trust by recruiting and training students from communities like Marion, in the hope that they will return home and spend their careers providing primary care where it’s desperately needed. It’s predicted that America will be short as many as 30,000 primary care doctors by 2025. And though around 20 percent of the U.S. population lives in rural areas, only 10 percent of physicians do. The pipeline was developed twenty-five years ago by John Wheat, a professor at the University of Alabama in Tuscaloosa. One evening, I joined Lee and Wheat for dinner at a seafood restaurant near campus as they discussed the depressing state of health care in the Black Belt over gumbo and fish tacos.
Wheat, who is sixty-five, is tall and grandfatherly. He sipped on sweet tea. He’s white — not born in the Black Belt, but his family moved there when he was young. He took to his rural surroundings — clearing the land, hunting rabbit, tending to horses and chickens — and eventually “married into a farm family.” He attended the University of Alabama School of Medicine, and worked in cities for a while, but he felt compelled to go back to the countryside.
Lee slurped a spoonful of gumbo. “We need doctors,” he said.
“Doctors from the community,” Wheat replied. “The uniform testimony from rural Alabama is: ‘We’re tired of missionaries and mercenaries. We need our kids in medical school.’ ”
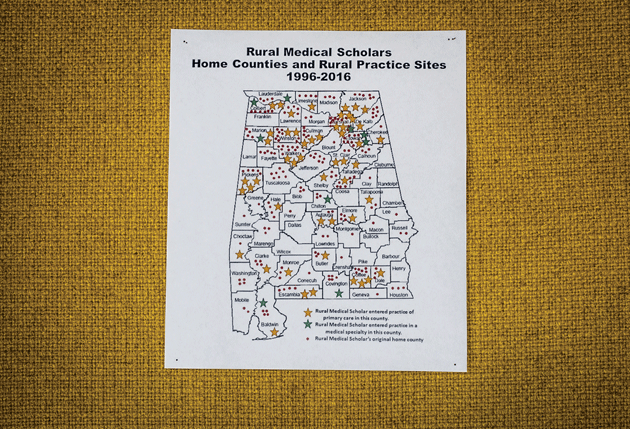
A map showing the home counties and practice sites of physicians who went through John Wheat’s pipeline program
Of the few physicians who pass through the Black Belt, most stay for only a few years, to do their good deed or satisfy recruitment packages that forgive school loans in exchange for working in an underserved area. There is another doctor providing care in Marion, who came from Pakistan, originally to fulfill a visa requirement, but he doesn’t live in town or conduct home visits. Lee had been trying relentlessly to recruit another doctor so that he could extend his clinic hours, but nobody was willing to make the commitment. “By their third year here, they’re interviewing every other weekend to go somewhere else,” he said.
When Wheat started the pipeline, in 1993, it was a summer program for high-school seniors from Alabama’s rural towns. They lived on campus in Tuscaloosa and took college-level chemistry and a writing seminar. The students met physicians, received support from peers and mentors, and were exposed to the steps for admission to medical school — all the advantages a child growing up in a city would have. “The farm kid who’s so rural he gets dizzy when he merges onto a four-lane highway? That’s the kid I want,” Wheat said. Several years in, to increase the number of black participants, he added an extra curriculum for the summer after high school that was aimed at minority students.
As the kids got older, Wheat made arrangements to secure their path in becoming physicians. If a student continued successfully in the pipeline and earned a minimum score on the Medical College Admission Test — lower than that required of other applicants — he or she would be guaranteed admission to the University of Alabama School of Medicine. Other rural students could apply to enter the pipeline for medical school by meeting the same academic standards. Wheat couldn’t secure free tuition, but these students were prioritized by the state for scholarships.
Since the program began, about 120 pipeline students have graduated from Alabama’s medical school. The first doctors entered into practice in 2004, and more than half have gone on to work in rural areas, compared with only 7 percent of their classmates. Studies have found that the addition of a single primary care physician to a community causes the local economy to grow by at least a million dollars per year; Wheat estimates that his program has delivered $320 million to poor rural towns — by generating medical revenue, creating employment, and revitalizing businesses.
But as we finished our dinner, my thoughts returned to Perry County, which hadn’t seen any of those gains. Recruiting from the area could be difficult, Wheat said, even when kids desperately wanted to sign up. I’d witnessed this obstacle when I’d attended a pipeline event at a school in Tuskegee. A bespectacled boy raised his hand to ask, “If we get into the program, how are we supposed to get to campus?” He didn’t know anyone with a car who would be willing to drive him to Tuscaloosa.

Customers at a gas station in Marion
Several years ago, when many of Wheat’s first students — only teenagers at the time they entered his orbit — had just finished their residency training, he drew up a map. He’d plotted red dots on their home counties and gold stars where they went on to practice. Looking at the results, he could see that there was a strip in the middle that was virtually blank. “They go around the Black Belt or cross over the Black Belt, but they don’t go into the Black Belt,” he said. For years, he realized, he’d been inadvertently omitting the very place he’d started from.
Many people in Marion wanted their hospital back, I said — would that help?
“They think the cure-all is to open another hospital,” Lee replied. “That’s the worst thing you can do! You’ve got to get physicians first.”
Wheat agreed. “The old theory of ‘Build a hospital, and they will come.’ Well, they don’t come!” The Black Belt, he had found, was a place where health care never seemed eager to go.
The standard treatment for tuberculosis is directly observed therapy — nurses watch over patients and give them each dose of medication, which can be upwards of two dozen pills at a time. Some of the drugs are as large as almonds. Early on, pills must be taken daily, and then they’re spaced out to twice a week, usually for another six to nine months. The treatment can make people feel awful, like they have the flu, and it can harm the liver, so patients are not allowed to drink alcohol.
Once Marion’s test results came in, the state health workers arduously tracked down people around the Hill. Barrett told me what this entailed: “You have to pick them up at the dumpster behind Hardee’s, and then drive them in your car with their head in your lap so no one would see them, and drop them off twenty yards away.” The health department bought a cell phone for a man who didn’t have one, so that his nurse could find him to give him his medication. Patients without cars were taken for rides where they wanted to go. Others received fresh groceries. On completion of their treatment, to increase compliance, they earned a hundred dollars. If they were desperate, health workers would try to hand them extra money. “Any scenario, any way we could get people to take their medicines,” Barrett said.
The state health workers left their homes in Montgomery for long stretches in order to work all hours on the Hill. They stayed at an inn in Marion and subsisted on takeout. “They care more about the patients than the patients care about themselves,” Barrett told me. But even if it seemed that way, all the health department’s efforts couldn’t fill the underlying void of care within the community. “Everything was reactive, not proactive,” Frances Ford said.
Wheat sees the spread of tuberculosis as the ultimate manifestation of an ongoing health care crisis in the region, characterized by mistreatment and neglect. “If we don’t respond, these are the things that happen,” he said. If a physician raised around Perry County had been working in Marion, he suggested, the outbreak would never have become so dire.
Last summer, as the state dispensed pills on the Hill, Wheat proposed to the University of Alabama a Black Belt Health Professional Scholars Program, in order to make it easier to bring students from the area into his pipeline. He hopes to further lower score requirements for their admission to medical school and to recruit students for a master’s in rural health — a one-year degree that can be stretched out to two years, for extra MCAT prep time. Courses would be open to anyone interested in working as a physician assistant, dentist, or physical therapist, which would deliver more people home to provide valuable medical services. “Over the long haul, this is the best way I can see to make a dent in this social circumstance that we’ve allowed to smolder here for two hundred years,” he said.
Wheat’s pipeline is paid for mostly by the state, which provides about $875,000 on a year-to-year basis; he also occasionally gets money from philanthropic foundations and federal grants. The school is committed to sustaining the program, but the fate of Wheat’s new proposal is less clear. His vision — $10 million spent over ten years and coordination across fifteen schools and campuses — may be too ambitious. “The idea of having physicians target the Black Belt, I think that’s tremendously timely and admirable,” Selwyn Vickers, the dean of the medical school, who was born in the Black Belt, told me. “But it’s not just getting individuals who want to go back. It requires broader infrastructure changes in the Black Belt. The state has to make the place attractive and build infrastructure so people want to go back. Otherwise, you’re not treating the cycle of poverty.”
In the meantime, Wheat has become ever more solicitous toward Black Belt students. He leaves his door open for advising sessions. “I keep a box of Kleenex,” he said. “Many tears have been shed in my office.” He has purchased textbooks for kids who couldn’t afford them and covered the costs of test fees. To beef up résumés, he has offered students jobs doing administrative work and postgraduate research.
One afternoon, I met Deanah Maxwell, a graduate of the program who is now thirty-seven. She entered the pipeline in its early years, as a teenager from Booker T. Washington High School in Tuskegee. (The current principal summed up her students’ circumstances to me: “Ninety-nine percent get free or reduced lunch.” She added, “They may have seen a shooting and stayed up late.”) When Maxwell arrived at the University of Alabama that first summer, she saw the possibility of a new life. “I’m a junior in high school, about to be a senior,” she recalled. “We didn’t do a lot of chemistry labs. This is a full-fledged lab! Folks are lighting Bunsen burners, and I was like, ‘What am I supposed to be doing?’ ”
She was enthralled, and persisted with premedical courses through college. She struggled with the MCAT — she took it twice before graduation, and both times failed to meet the pipeline’s minimum score requirement for rural students — so Wheat found her a job as a research assistant, which gave her access to prep courses and study materials. On her third try, she passed. When she finished medical school, she worked in southern Alabama for a while before returning two years ago to Tuskegee, where she intends to stay.
Tuskegee, due east of Marion, is flat with green and yellow fields; in the center of town, near the site of the infamous syphilis study, is Maxwell’s clinic. When I visited, she introduced me to one of her patients, Roberta Crenshaw, who sat in the exam room wearing a colorful floral shirt and bright red pants. I asked what she remembered of Maxwell’s return. “I was so happy to see her!” she told me. “A home person. Somebody that grew up here. I know her father, I know her mother.” Beaming, Crenshaw turned to Maxwell. “I’d been waiting fifteen years for you to come home!”
Where a doctor comes from matters to the place she works. Yet results of the MCAT — a grueling, eight-hour exam — can be entered into admissions algorithms such that applicants to medical school are axed before a human being even considers their background. When I asked Wheat whether any of his doctors-in-training resented his helicoptering or were irked that he was lowering the score bar for them, he replied, “No, the minority population that comes to us have found it a relief that someone understands that these quantitative measures are not measures of their potential.” He continued, “Now, I’ve certainly had the Caucasian population question lowering the quality. And I say, ‘Quality of what?’ ” Black Belt students, he went on, “bring an intention and an identity with an underserved population that it is a mission of our medical school to serve.”
The purpose of doctors, after all, is to tend to patients’ ultimate needs. Increasing the supply of primary care physicians is linked to lower mortality rates; after compiling data from studies across different parts of the country, a group of public health researchers found that by adding one more doctor for every 10,000 people, as many as 160,000 deaths per year could be averted. When the same researchers considered race as a factor, this benefit was found to be four times greater in the African-American population than among white people. Studies have also observed that the availability of primary care significantly reduces health disparities that result from income inequality.
Outside Alabama, a handful of other programs have tried to correct the distribution imbalance of physicians in the United States. At Thomas Jefferson University, in Philadelphia, a rural health pipeline has been targeting poor, mostly white areas of Pennsylvania and Delaware for forty years. The University of Missouri and the University of Louisville run similar initiatives. Last year, the City University of New York welcomed its first class of medical students; the school intends to train doctors to care for communities in the Bronx and Harlem — which, in health care terms, have more in common with Perry County than with most of Manhattan.
Yet for the most part, medical schools are focused on selecting high achievers rather than grappling with inequality. While this has been an effective strategy in advancing American medicine, large swaths of the population perpetually go without proper health care, and it’s hard not to see — as Lee, Wheat, and Ford do — that the lack of attention to places like the Black Belt creates the conditions for an outbreak of tuberculosis, along with scores of other diseases.
When I posed this dilemma to Robert Alpern, the dean of Yale Medical School, he conceded that interest in diversity doesn’t always serve its true purpose. “We all offer scholarships to steal students from other schools, to save our own skin, but in fact we don’t do anything for the country,” Alpern told me. “All we do is shuffle these students around.” A more comprehensive solution, he said, would be beyond the university’s capacity.
George Daley, who became the dean of Harvard Medical School in January, spent his first month on the job creating a diversity task force to address gaps in racial and socioeconomic representation, at a moment when only about 5 percent of America’s medical school graduates are black. But he won’t be lowering academic standards to bring in applicants who wouldn’t otherwise be accepted. “We’re in a position of taking absolutely stellar students and aspire to train the best doctors,” he told me. And while Harvard has a center devoted to primary care, he said, “I’m not sure our role is to prespecify where you should go. We try to inspire them to go into public service and try to encourage people to work in diverse communities.” He added, “Harvard can’t be all things to all people.”
The state health department’s efforts in Marion were astounding, and they seemed to be effective. For a while Barrett believed that the spread of tuberculosis had been controlled. But when I checked in with her again in the spring, she told me that four cases had been discovered since I’d been to town, and that she wasn’t sure when the outbreak would be over. “It’s not looking good,” she said.
Lee is still on the lookout for symptoms. He has yet to find another doctor to join his practice, but he is hoping that his son, who just finished medical school, will take the job. “I’m getting old,” Lee said. “If my son doesn’t come back to take over the clinic, I’m going to work until I’m sixty, and I’m done.”
One evening, I drove along the route that leads from Marion to the hospital in Greensboro. A doctor there named Dana Todd had invited me to visit her house. The night was foggy and the road curved; even with my high beams on, I couldn’t see more than a foot or two ahead. The thought of an ambulance trying to navigate the blind turns was terrifying.
When I arrived, Todd greeted me at her front door wearing a sleek red dress and magenta lipstick that popped against her dark skin. She was tall with short hair. “This feels really weird,” she said as she invited me inside. I saw what she meant: the whole house was empty. “The movers came while I was at work,” she explained. As it happened, it was her last night in Greensboro. The next morning she was moving to Durham, North Carolina, to start a new job at a primary care clinic affiliated with Duke University.
Wheat had told me that Todd was “the poster child” of the Rural Health Leaders Pipeline. She flew through the high school program into the minority summer course and then earned a master’s degree in rural community health as well as a spot in medical school. She also returned as a counselor. After finishing her training, she came back to live and work in her hometown as a family doctor — exactly as Wheat had hoped. Yet she couldn’t stay. “I did three and a half years here,” Todd said. “But my intent was to do thirty.”
She decided to take me to a Mexican restaurant, since she had no furniture for us to sit on. I hopped in her car, and as she took off and started talking at a fast clip, she struck me as more of a city person than someone who grew up in the rural South. Passing the town’s private school, she said, “It’s ninety-nine percent white. I’ve never known a single black person to go to that private school.” In Marion too, the public schools are filled almost entirely with black children from poor families, and the white kids attend a private school in town. This is the default scenario throughout the Black Belt counties of Alabama, leaving the public schools homogeneously black and severely underfunded.
Todd has a son, who is seven, and he had been going to the same public elementary school that she attended. She was worried that his prospects would be limited if they remained. As he gets older, she wants him to meet a more diverse group of people — a different group — and have access to greater opportunities, the ones that had yet to come to the Black Belt. “That’s the most unfortunate part about living here,” she told me. “We’re not progressing at the same rate as everything else around us.” She sighed. “We’re just kind of stuck.”
At the restaurant, we slid into a booth. “This is one of the few places in town I can come and not see eight people I know,” Todd said. People have come up to her at church and asked for medication refills, stopped her in the grocery store for their test results, knocked on her door at night with medical queries. Being the only doctor in town, she felt like she was at work all the time.
And in her personal life, she was isolated. Most of her peers lived in cities with greater employment potential. Few of her childhood friends with professional degrees had returned to Greensboro. Her mother had worked in a sewing factory and her dad was a truck driver; she was the first in her immediate family to graduate from college. “People think you are a millionaire,” she told me. “To make six figures in a town where people don’t earn that sort of living.”
Now she was discouraged by a forsaken quality of her hometown. “One person just can’t do it,” she said. “It sounds very nice, but one person cannot change everything.”
I thought of Marion, still in jeopardy. Later, I called Marsha White to find out how she was doing. When she answered, she sounded stressed, and said that she was taking care of her grandson. I could hear the baby crying in the background. But as we talked, I learned the real reason for the strain in her voice. She told me that, months after she thought the town had come out of its sickness, she had been reinfected with tuberculosis.




































































































